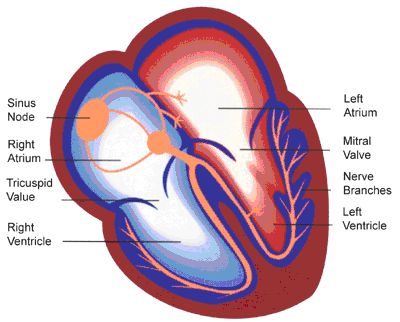
Every heart beat is initiated by the sinus node in the right atrium, sending an electrical signal that spreads to the left atrium (these are the 2 upper chambers of the heart) and the connecting points of the ventricles (lower chambers). The atria contract first, followed by the ventricles a fraction of a second later. This is illustrated below.
If the atria do not receive correct instructions to contract from the sinus node they begin to quiver, or fibrillate. This is known as atrial fibrillation and the heart beat becomes irregular. There is still enough blood going to the ventricles to supply the rest of the body. Nearly 50,000 patients are diagnosed with the condition each year and it is more common in older adults. The risk of developing atrial fibrillation doubles with each decade after 50 years of age.
The sinus node however, can malfunction in a variety of conditions. These include coronary heart disease, valve disease, thyroid disease, diabetes, infection, electrolyte abnormalities, hypothermia and drugs such as alcohol. The condition is idiopathic in up to 9% of cases.
The main symptom of atrial fibrillation is palpitations. This may also be accompanied with shortness of breath, chest pain and dizziness. Many patients however, are asymptomatic and the condition is discovered incidentally.
The diagnosis of atrial fibrillation is confirmed with an ECG that will show the heart's irregular rhythm. This is illustrated below.

Blood tests for routine monitoring of electrolytes and thyroid function tests should be performed. If the patient suffers only occasional symptoms, it would be necessary to record the electrical activity of the heart over 24 hours with an ambulatory ECG monitor. A chest X-ray and echocardiogram should be performed to help elicit an underlying cause of the atrial fibrillation, e.g. infection or valvular pathology.
The main aims for treatment of atrial fibrillation are:
- Treat any underlying cause e.g. thyroid disease, infection.
- To restore a regular heart rhythm- this can be done by electrical DC Cardioversion that shocks the heart back into a normal rhythm. The longer the atrial fibrillation goes on however, the less successful this is likely to be as the heart adapts to its new rhythm. Certain medications can also be used to achieve chemical cardioversion and restore a regular rhythm with this.
- To prevent thromboembolism, or clot formation. The main risk of atrial fibrillation is that of clot formation in the left atrium. These may be swept away and lodge in a small artery in other organs, e.g. the brain to cause a stroke. Patients with the condition are up to 6 times more likely to have a stroke than those in a regular rhythm. However, appropriate risk stratification and blood-thinning treatment can be used e.g. aspirin, warfarin, dabigatran, to reduce the chances of this happening. Sometimes atrial appendage closure devices are used to further reduce the chances of clot formation. This is performed in a similar way to cardiac catheterization under X-ray and echocardiographic guidance.
- To control the heart rate with medication, e.g. beta-blockers, calcium-channel blockers or digoxin.
If control of the atrial fibrillation is still difficult and the patient is asymptomatic, another option is to ablate the abnormal electrical pathways using a procedure called radiofrequency ablation. Sometimes a pacemaker may be required to control the heart rate may the most appropriate therapeutic option. Your cardiologist will best advise you on the management strategy.
Contact Us
01494 867 616
info@chilternheart.com
To book an appointment click here
